[Translate to En:](Kopie 1)
(copy 2)
Functional pediatric precision oncology
To help pediatric patients suffering from tumors that either lack actionable therapeutic targets or become refractory to treatment, we are pursuing the following research approaches:
The aim of the Translational Drug Screening Unit (TDSU) is to complement molecular genetic analyses with functional analyses in the form of high-throughput drug screens. To that end, we use cells from tumor biopsies of patients from the INFORM study. We then culture these cells as three-dimensional multicellular spheroids (miniature tumors) and, within a few days of tumor resection, test them for sensitivity to a large number of clinically relevant anticancer therapeutics, thereby generating a drug sensitivity profile of each tumor sample. Additionally, we aim to establish molecularly defined long-term cell cultures from these samples to increase the number of available clinically relevant patient-derived models.
In parallel, we investigate resistance mechanisms in various pediatric nervous system tumors (e.g., neuroblastomas and gliomas), with a special focus on highly treatment-resistant tumor subtypes. With the identification of mechanistic vulnerabilities, we aim to create novel treatment options for these tumors. Promising therapy approaches are rapidly transferred to in vivo testing in our zebrafish early larvae xenograft model.

Spotlight - Group Oehme
Creation of drug sensitivity profiles in INFORM
The international multicenter INFORM program addresses an unmet medical need by providing comprehensive molecular next-generation sequencing (NGS) information, including areawide whole-genome sequencing, whole-exome sequencing, RNA sequencing, and 850k DNA methylation profiling for relapsed/refractory pediatric cancer patients.
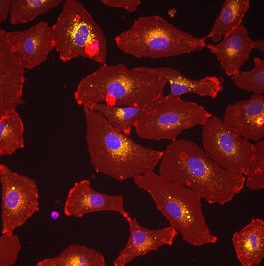
The main focus of the Translational Drug Screening Unit (TDSU) is translational research from bench to bedside and back. Our aim is to identify more therapeutic options for pediatric cancer patients by integrating functional single and combination drug response data with the well-established INFORM molecular profiling analysis. To this end, we implemented drug sensitivity profiling on microtumors generated from fresh tumor specimens of INFORM patients (Peterziel et al., 2022). These microtumors are three-dimensional (3D) heterogeneous multicellular spheroids under serum-free conditions to preserve cellular interactions and cell-derived extracellular matrix composition. Drug screening is performed within 2-7 days after tumor resection/biopsy from the patient, using clinically relevant anticancer therapeutics to generate a drug sensitivity profile (DSP) of every individual tumor. Hits are identified based on outlier sensitivity within the (constantly expanding) DSP cohort and with consideration of clinically relevant parameters, e.g., effect at clinically achievable concentrations. In close collaboration with other KiTZ groups, we additionally employ our platform to generate DSP data on pediatric tumor cell lines, patient-derived long-term cell cultures and PDX tumor cell reisolates.
We use pediatric cancer zebrafish (Danio rerio) embryo models to investigate and monitor tumor growth and progression at the single-cell level and to validate the cell culture results. The zebrafish models serve as a medium- to high-throughput approach for in vivo drug screening to identify potential therapeutic strategies for the treatment of children with relapsed cancers. Xenograft models from both established cell lines and patient-derived tissue samples (zPDX) are employed to evaluate and predict therapeutic response.
The aim of these projects is the identification of actionable cellular alterations in pediatric nervous system tumors (neuroblastoma, medulloblastoma, glioma, ependymoma) via high-throughput drug screening. We use various tumor models, such as patient-derived short- and long-term cultures and established cell lines, to investigate, for example, whether anticancer drugs targeting the epigenome could be a therapeutic option for children with diffuse midline glioma harboring H3 mutations who present with a very poor prognosis. In the case of treatment-resistant neuroblastomas, we explore how inhibition of cell surface receptors and drug efflux pumps and interference with matrix metalloproteinases can overcome chemotherapy resistance. An additional focus of our studies is the lysosome, a cellular organelle responsible for the degradation of cellular macromolecules. In the case of treatment-resistant neuroblastoma, we showed that a member of the histone deacetylase (HDAC) family, HDAC10, promotes autophagy as well as the secretion of drugs via lysosomal exocytosis (Oehme et al. 2013, Ridinger et al. 2018). We further demonstrated that broad-spectrum HDAC inhibitors such as panobinostat and vorinostat modulate autophagy in neuroblastoma and that the combination of these HDACis with autophagy inhibitors such as chloroquine effectively kills neuroblastoma cells (Koerholz et al. 2021).
We have identified the HDAC member HDAC8 as a therapeutic target in neuroblastoma. Inhibition of HDAC8 promotes the differentiation of aggressive neuroblastoma cells in vitro and in vivo (Oehme et al. 2009, Rettig et al. 2015). Additionally, inhibitors of the receptor tyrosine kinase ALK, which we identified as a potentially synthetic lethal target in a kinome-wide RNAi screen, proved to be synergistic combination partners of HDAC8 inhibitors. The simultaneous inhibition of HDAC8 and ALK signaling blocks tumor-relevant signaling pathways such as ERK signaling which effectively induces cell death in neuroblastoma cells (Shen et al. 2018). However, our studies also show that a subset of cells escape HDAC8 inhibitor treatment. We are currently investigating how these treatment-surviving cells differ in their gene expression profile from HDAC8 inhibitor-sensitive cells to systematically screen for actionable targets in HDAC8i-resistant cells. One potential way of killing such resistant cells is the simultaneous inhibition of HDAC8 and HDAC10 via highly selective HDAC6/8/10 inhibitors such as TH34 (Kolbinger et al. 2018).
Peterziel H, Jamaladdin N, ElHarouni D, Gerloff XF, Herter S, Fiesel P, Berker Y, Blattner-Johnson M, Schramm K, Jones BC, Reuss D, Turunen L, Friedenauer A, Holland-Letz T, Sill M, Weiser L, Previti C, Balasubramanian G, Gerber NU, Gojo J, Hutter C, Øra I, Lohi O, Kattamis A, de Wilde B, Westermann F, Tippelt S, Graf N, Nathrath M, Sparber-Sauer M, Sehested A, Kramm CM, Dirksen U, Kallioniemi O, Pfister SM, van Tilburg CM, Jones DTW, Saarela J, Pietiäinen V, Jäger N, Schlesner M, Kopp-Schneider A, Oppermann S, Milde T, Witt O, Oehme I. Drug sensitivity profiling of 3D tumor tissue cultures in the pediatric precision oncology program INFORM. NPJ Precis Oncol. 2022 Dec 27;6(1):94.
Rösch L, Herter S, Najafi S, Ridinger J, Peterziel H, Cinatl J, Jones DTW, Michaelis M, Witt O, Oehme I. ERBB and P-glycoprotein inhibitors break resistance in relapsed neuroblastoma models through P-glycoprotein. Mol Oncol. 2022 Oct 1. doi: 10.1002/1878-0261.13318. Epub ahead of print.
Gatzweiler C, Ridinger J, Herter S, Gerloff XF, ElHarouni D, Berker Y, Imle R, Schmitt L, Kreth S, Stainczyk S, Ayhan S, Najafi S, Krunic D, Frese K, Meder B, Reuss D, Fiesel P, Schramm K, Blattner-Johnson M, Jones DTW, Banito A, Westermann F, Oppermann S, Milde T, Peterziel H, Witt O, Oehme I. Functional Therapeutic Target Validation Using Pediatric Zebrafish Xenograft Models. Cancers (Basel). 2022 Feb 8;14(3):849.
Müller M, Rösch L, Najafi S, Gatzweiler C, Ridinger J, Gerloff XF, Jones DTW, Baßler J, Kreth S, Stainczyk S, Frese K, Meder B, Westermann F, Milde T, Peterziel H, Witt O, Oehme I. Combining APR-246 and HDAC-Inhibitors: A Novel Targeted Treatment Option for Neuroblastoma. Cancers (Basel). 2021 Sep 5;13(17):4476.
Körholz K, Ridinger J, Krunic D, Najafi S, Gerloff XF, Frese K, Meder B, Peterziel H, Vega-Rubin-de-Celis S, Witt O, Oehme I. Broad-Spectrum HDAC Inhibitors Promote Autophagy through FOXO Transcription Factors in Neuroblastoma. Cells. 2021 Apr 24;10(5):1001.
Wrobel JK, Najafi S, Ayhan S, Gatzweiler C, Krunic D, Ridinger J, Milde T, Westermann F, Peterziel H, Meder B, Distel M, Witt O, Oehme I. Rapid In Vivo Validation of HDAC Inhibitor-Based Treatments in Neuroblastoma Zebrafish Xenografts. Pharmaceuticals (Basel). 2020 Oct 27;13(11):345.
Kolbinger FR, Koeneke E, Ridinger J, Heimburg T, Müller M, Bayer T, Sippl W, Jung M, Gunkel N, Miller AK, Westermann F, Witt O, Oehme I (2018) The HDAC6/8/10 inhibitor TH34 induces DNA damage mediated cell death in human high-grade neuroblastoma cell lines. Arch Toxicol. 2018 Aug;92(8):2649-2664.
Shen J, Najafi S, Stäble S, Fabian J, Koeneke E, Kolbinger FR, Wrobel J, Meder B, Distel M, Heimburg T, Sippl W, Jung M, Peterziel H, Kranz D, Boutros M, Westermann F, Witt O, Oehme I (2018) A kinome-wide RNAi screen identifies ALK as a target to sensitize neuroblastoma cells for HDAC8-inhibitor treatment. Cell Death & Differentiation. Dec; 25(12): 2053–2070.
Ridinger J, Koeneke E, Kolbinger FR, Koerholz K, Mahboobi S, Hellweg L, Gunkel N, Miller AK, Peterziel H, Schmezer P, Hamacher-Brady A, Witt O, and Oehme I (2018) Dual role of HDAC10 in lysosomal exocytosis and DNA repair promotes neuroblastoma chemoresistance. Sci Rep. 2018 Jul 3;8(1):10039.
Bingel C, Koeneke E, Ridinger J, Bittmann A, Sill M, Peterziel H, Wrobel JK, Rettig I, Milde T, Fernekorn U, Weise F, Schober A, Witt O, Oehme I (2017) Three-dimensional tumor cell growth stimulates autophagic flux and recapitulates chemotherapy resistance. Cell Death Dis 8: e3013.
Rettig I, Koeneke E, Trippel F, Mueller WC, Burhenne J, Kopp-Schneider A, Fabian J, Schober A, Fernekorn U, von Deimling A, Deubzer HE, Milde T, Witt O, Oehme I (2015) Selective inhibition of HDAC8 decreases neuroblastoma growth in vitro and in vivo and enhances retinoic acid-mediated differentiation. Cell Death Dis 6: e1657.
Oehme I, Lodrini M, Brady NR, Witt O (2013) Histone deacetylase 10-promoted autophagy as a druggable point of interference to improve the treatment response of advanced neuroblastomas. Autophagy 9(12):2163-2165.
Oehme I, Linke JP, Böck BC, Milde T, Lodrini M, Hartenstein B, Wiegand I, Eckert C, Roth W, Kool M, Kaden S, Gröne HJ, Schulte JH, Lindner S, Hamacher-Brady A, Brady NR, Deubzer HE, Witt O. (2013) Histone deacetylase 10 promotes autophagy-mediated cell survival. Proc Natl Acad Sci U S A 110(28): E2592-2601.
Oehme, I., Deubzer, H. E., Wegener, D., Pickert, D., Linke, J. P., Hero, B., Kopp-Schneider, A., Westermann, F., Ulrich, S. M., von Deimling, A., et al. (2009). Histone deacetylase 8 in neuroblastoma tumorigenesis. Clin Cancer Res 15, 91-99.
- Celikyürekli, Simay (Ph.D. student)
- Digel, Lea (student assistant)
- Friedenauer, Aileen (technical assistant)
- Gatzweiler, Charlotte (MD student)
- Gerloff, Xenia (student assistant)
- Herter, Sonja (Ph.D. student)
- Hugo, Anette (technical assistant)
- Körholz, Katharina (MD student)
- Loboda, Anna (Ph.D. student)
- Melero Emperador, Marta (Ph.D. student)
- Mohr, Jacqueline (student assistant)
- Müller, Michael (MD student)
- Najafi, Sara Dr. sc. hum. (Post-Doc)
- Oehme, Ina PD Dr. phil. nat. (group leader)
- Peterziel, Heike Dr. rer. nat. (staff scientist)
- Rösch, Lisa (Ph.D. student)
- Salem-Altintas, Rabia (MD student)
- Seiboldt, Till (MD student)
- Stroh-Dege, Alex (technical assistant)
- Weidmann, Marko (technical assistant)
- Zeiser, Constantia (MD student)

Postal address:
German Cancer Research Center
CCU Pediatric Oncology / G340
Im Neuenheimer Feld 280
D-69120 Heidelberg
Germany